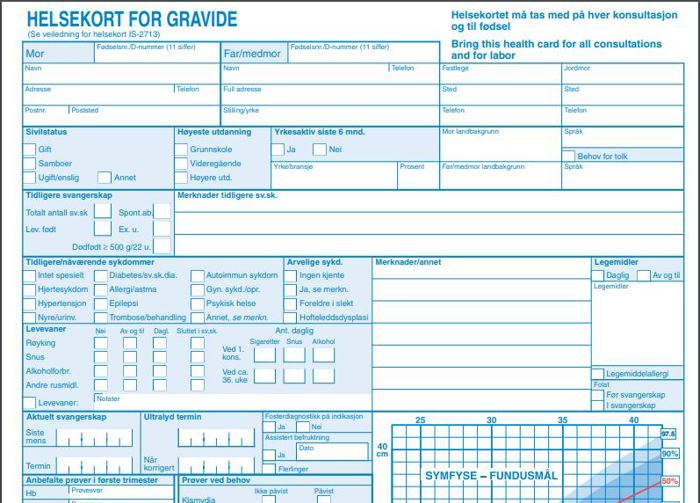
What is an antenatal health card?
The antenatal health card is a medical record on paper and a link between you, the doctor, the midwife and the hospital. The card ensures that everyone receives the same information about you and your child’s health, as well as any special needs you may have. You decide what information you wish to provide.
During your pregnancy, you must take your card with you to all consultations and examinations with your GP, midwife, hospital and other healthcare services you come into contact with. You must also take your card to the maternity ward when you go there.
Tell your doctor/midwife if you have lost your health card. If you forget to take it to a check-up, it is important that you make a note of any entries and information on the card later.
Mandatory information in the health card
The information given in the health card will be important for your pregnancy and birth. Information on the following must be filled in:
Mother and father/co-mother
- Address
- Marital status
- Education
- Profession
- Place of work
- Country background
- Language
- Name and phone number of your GP and midwife
If you are not married to the child's biological father, you should check the box to indicate whether a paternity declaration (in Norwegian) has been completed during the pregnancy.
History
- all previous pregnancies
- births
- spontaneous abortions
- Past or present illnesses which could affect you and/or your child.
You may also be asked about the birth of your mother and/or sister, because there may be genetic links.
Conditions requiring extra support, such as
- diabetes
- epilepsy
- metabolic diseases
Conditions which the healthcare service wishes to assess, including
- cardiovascular diseases
- kidney disorders
- asthma and allergies
- gynecological disorders
- congenital hip defects
- blood clotting (thrombosis)
- high blood pressure (hypertension)
- mental illness
Medicines
Information about whether you
- are taking any over-the-counter or prescription medication
- have drug allergies
Your lifestyle
Information about your lifestyle
- diet and dietary supplements
- physical activity
- employment situation
- use of tobacco, alcohol and other drugs
You will be asked about the number of cigarettes you smoke per day to determine the level of risk that this poses to you and your child.
Due date
- Estimated due date (corrected following determination of the due date through an ultrasound examination)
Routine examinations and any needs regarding other tests
Various routine examinations and tests will be carried out during your pregnancy.
Measurements of the mother
- symphysis-fundus measurement (measurement of the uterus, done on the outside of the abdomen)
- blood type
- blood pressure
- height
- weight and BMI
Measurements of the fetus
Fetal diagnostics, including the fetus’s
- heartbeat (fetal sound)
- movements
- how the fetus is lying/presented
Consultations
All examinations that you have during your pregnancy will be recorded, so that the midwife and other medical professionals know what kinds of treatment you have received. A note will also be made as to whether you have been given guidance concerning breastfeeding and attended a course aimed at preparing you for childbirth/parenting.
Birth location and health centre
Your midwife and GP will help you choose where to give birth and enter your birth location onto the health card. If you need the companion service, this should be noted. The health centre, where you will receive follow-ups after you have had your baby, will also be noted.

Antenatal checks and tests
All pregnant women are entitled to antenatal care. The service is free and intended to ensure that you receive the best possible care and guidance during and after your pregnancy.
Illustration: Lev Dolgachov / Mostphotos
Need more follow-ups?
If you need extra follow-ups, it is very important that your midwife or doctor receives information about this.
This may be information about social circumstances, such as that you or the father/co-mother
- are unemployed
- need financial support
- have language difficulties
or physical/mental circumstances, such as
- disease, health problems
- disability
- experience of violence and/or past abuse
- traumatic experiences from the health service, previous pregnancies or childbirth
What do the abbreviations mean?
The list below explains the meanings of some of the terms on your antenatal health card, but you do not need to know or understand these terms. Ask your midwife or doctor if you are unsure of anything.
|
Term |
Meaning |
|
AB0 |
Your blood type is recorded as: A, B, AB or O. |
|
ABU |
Asymptomatic bacteriuria. Refers to levels of bacteria in the bladder and urine. |
|
P/Alb |
Protein/albumin (egg white) in urine. |
|
BT |
Blood pressure. |
|
Ex. u. |
Ectopic pregnancy (pregnancy outside the uterus). |
|
Ferritin |
Blood test which tells you your iron level. |
|
Fl/min. |
Fetal heart rate (fetal heartbeat) per minute. |
|
Position |
How the fetus is presented or oriented. H/S/T/F/B are codes for the normal cephalic, breech, transverse (where the foetus is lying laterally) position of the fetus and whether the head has become engaged. |
|
Glucose load |
Test which shows how your body copes with the intake of a specific amount of sugar (glucose). |
|
Hb |
Haemoglobin count (blood count, test for possible anaemia). |
|
HIV |
Test results from HIV test. |
|
Medication - |
No regular medication. |
|
Medication + |
Use of drugs, including iron, vitamins and folate. |
|
MRSA |
Resistant bacteria known as methicillin-resistant Staphylococcus aureus. |
|
RH-D |
Your blood type or that of the foetus may be Rh-positive or Rh-negative. |
|
Syphilis |
Syphilis sample. The date on which the sample was taken and the test result is recorded here. |
|
Symphysis-fundus measurement |
Assumed distance from the upper part of the pelvic bone to the top of the uterus. Stated in centimetres and noted on the diagram. |
|
Due date |
Anticipated date of birth; one based on your menstrual cycle and one based on an ultrasound examination. Corrected due date will be the due date based on an ultrasound examination. |
|
Week |
How far you have progressed in your pregnancy. Stated in full weeks + days. |
|
Oedema |
Water accumulations in the body, for example in the legs. |
|
+ |
Traces found. |
|
- |
No findings. |